
Nurses on the front line
Special to the Times | Bazhnibah
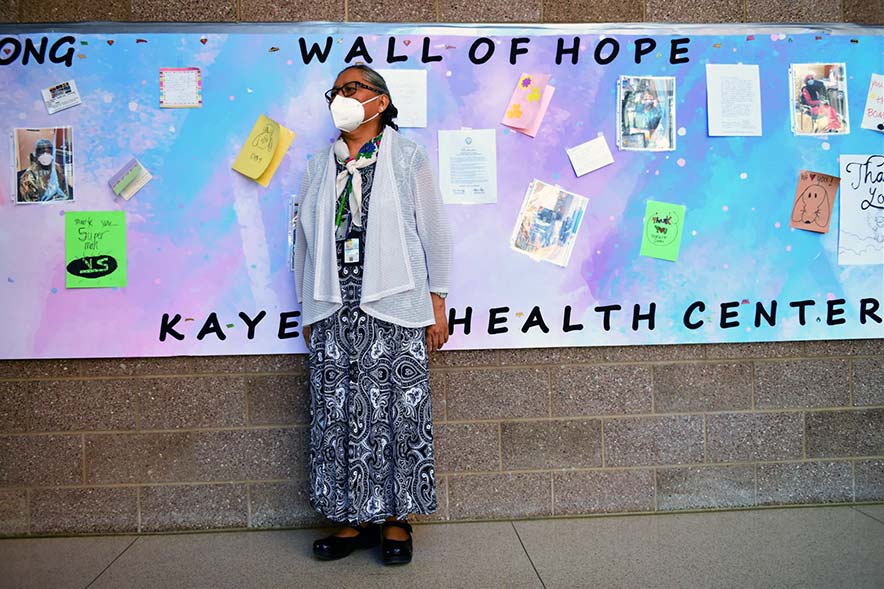
Registered Nurse Wanda Begay stands proudly in front of the Kayenta Health Center’s “Wall of Hope” with cards and notes of appreciation from patients and staff.
By Ruth Kawano
KAYENTA
“I never thought it would come here, not here on the reservation.” She first heard about the coronavirus (COVID-19) on TV in January 2020. “It’s all the way across in China!”
This nurse tearfully expressed what it was like in the beginning when it came to the Navajo Nation. Another nurse detailed the preparation of staff and protocols before the virus hit close.
A chief nurse executive used her leadership skills to help create innovative solutions for her staff and patients. These professional registered nurses voiced early experiences, painting painful scenarios of patients and sometimes a whole family suffering with COVID-19 as they stepped into the Kayenta Health Services Emergency Department.
Patients started showing up in late February. The coronavirus, which causes COVID-19, is a novel virus that has affected millions throughout the world – more than 5 million people as of this writing with more than 340,000 deaths.
In March, Navajo leaders named the virus Dikos Ntsaaígíí-19. COVID-19 affects the lungs and its airways. The coronavirus is a lethal virus, easily infecting others.
On the Navajo Reservation, currently there are more than 4,500 positive COVID-19 cases with 2,000 recovering and 153 who died. COVID-19 continues to spread.
Education to prepare
Knowing about the coronavirus in January and February of this year, the Kayenta Health Center’s nursing staff started preparing with education.
“First, I mentally prepared myself to be the cheerleader and quality leader for my team and co-workers,” said Kathleen Whitehorse, an RN in the Emergency Department. “We maintained our daily positive quotes that we already had in place before COVID-19 and I had to be a positive and strong leader in the face of COVID-19.”
As a public service, the Navajo Times is making all coverage of the coronavirus pandemic fully available on its website. Please support the Times by subscribing.
How to protect yourself and others.
Why masks work. Which masks are best.
Resources for coronavirus assistance
She didn’t know if this virus would be like Ebola, another killer virus responsible for over 20,000 deaths worldwide in 2014. Nurses had questions about the coronavirus. Would it really come to the Navajo Reservation? Soon it wasn’t an “if” but a “when.”
The team set up scenarios and practiced donning and doffing PPEs – personal protective equipment – like masks, gowns, face shields, gloves, etc. They also learned as much as they could about the virus.
Eileen Russell, RN, a supervisory clinical nurse in the Emergency Department, said, “In preparation, I reminded myself of why I became a nurse and that I will treat others like I would want to be treated if I were the patient or family member. “I also prayed for guidance in matters unfamiliar to me and that I will not be fearful of what comes before me and to make the best decision with the best resources available to me,” she said.
She prepared her ED nursing staff to treat customers to the best of their abilities. She knew that residents had to be educated about the virus in careful terms because the average person does not know what a virus is and how it causes illness.
A chief nurse executive at the Kayenta Service Unit Health Center, Wanda Begay oversees the nursing department. To prepare her staff, Begay ensured adequate supplies and that every nurse was educated about the types and uses of PPE and the virus.
Staffing was a big challenge. To begin with, the nursing vacancy rate was high at 65%. She had to get extra nurses. In the beginning of the pandemic, she got contract nurses and volunteers such as Team Rubicon, a group of military veterans who help in disaster management around the world.
They also received help from FEMA and Doctors Without Borders. These workers went to communities to teach about the virus, including masking, social distancing, virus shedding and even grocery shopping.
All resources were much needed and appreciated by all in Kayenta. In the beginning, the virus also caused fear and anxiety among staff.
Staff was afraid to go into the ED for lab specimen transport, housekeeping and supply management. They were educated by professionals to lessen their fears. It was important for nurses to know as much about the virus as possible. Begay said, “My expectation was to make sure our team followed our plan on what to do if a COVID-19 patient walked into our emergency room doors – they were donned in PPE and the patient got a mask immediately.”
Then other protocols were followed. The more staff followed the protocols, she said, the easier it got.
In late February, the KHC got a patient with a high fever and a dry, unexplainable cough. “We weren’t sure (if this was a COVID-19 patient) but with the high fever we had heard about, it got real,” Begay said. “Maybe this was a COVID-19 patient!
“We weren’t sure because we had a lot of flu patients with similar signs and symptoms and there was no test yet to see if affected from the coronavirus,” she said.
Initially it took five to seven days to get test results back, so it was challenging for staff to know if patients had COVID-19 or not. Later in March, they started testing. However, she noticed that the ED situation was harder to deal with and that nurses were stressed.
“The more we found out about the virus, the harder it was to see what every patient endured with the hardship of what this virus was doing to their bodies,” Begay said. Knowing that the patient and family were experiencing all the pain and suffering was much to bear.
As a nurse caring for patients, she knew that the patient could not have family around and had to be alone. “I let them know how I feel, I touch their shoulder, I ask them if they have any questions and I tell them about what the virus is doing to their lungs in layman terms,” Begay said.
She saw how her patients had difficulty breathing and even more difficult was seeing children suffering. Witnessing a whole family with the illness and seeing their oxygenation dwindle was devastating. Nurses here had not dealt with anything like this before!
Because the virus is very evasive, virulent and new to all, nurses realized that education is important. Even scientists, virologists and doctors still do not know everything about COVID-19 and how it seems to travel.
Currently there is no cure or vaccine. An antiviral is said to be in clinical trials the past week. From reports, world scientists are working around the clock to develop treatments.
Apart from patient care, medical supplies and PPE were getting harder to get from manufacturing centers. Staff decided to use Tyvek material from a home improvement store to start making gowns, which could be wiped down and reused. They got rolls of this materials and staff started cutting and sewing makeshift gowns.
Rapid test kits and machines came much later. These kits are used for point-of-care testing for COVID-19. In the past staff had to transport tests to a lab as far away as Phoenix, some 300 miles away or a five-hour drive, for a five to seven day turnaround for test results, sometimes even longer. ED staff also started using industrial face shields for added protection. CAPRs (controlled air purifying respirator) were ordered by the staff, but not received yet. This is a new PPE, which can be a face shield helmet, or a shroud with a helmet and face shield which goes around the head and upper body.
Other changes included establishing a nurse call line where patients could find answers to their questions in English and Navajo. The inpatient unit has become an extended ED overflow unit for positive COVID patients who were waiting for transfer to an outside hospital or stable patients that needed oxygen, intravenous fluids, medications, and monitoring. An outside curbside drive-through is set up for follow-up by recovering patients.
Most of the KHC clinics except for a few have been closed.
Lessons learned after two months, Whitehorse said, include that she “became a stronger advocate for the care of patients, more attentive in helping them understand COVID-19 signs and symptoms. “I helped them think more positively, urged them to stay strong and let them know how important they were to me,” she said. “COVID-19 is a strong virus. Nurses can be strong mentally, emotionally, physically, too, we let our inner leadership qualities take over. “We got this,” she said. “We can overcome adversity because we are RNs.”
Russell stressed that any nurse who comes to the Navajo Area must understand the remoteness and culture. “Kayenta is a remote area and families live with extended family members,” she said. “There are areas of no electricity, heat or plumbing and it makes our education to wash frequently difficult to implement in family homes.
“New RNs and nursing students should not fear coming here, there is much to learn here, although we may not have all the modern technology as in the urban areas,” she said. “We do more hands-on care and have to do a lot of critical thinking.”
Begay found that training staff to work in different areas and education in the clinics and directing traffic was important. “Nurses had to work outside in a tent and at curbside,” she said. “Nurses and support staff manned the established nurse call line and used the Diné/Navajo language to answer questions on COVID-19 and inform callers on signs and symptoms, testing, and self-quarantine.”
More nurses are needed in the rural communities on the Navajo Nation. “We need to recruit and seek more resources for scholarship and education to send our children to schools,” Begay said. “There are going to be more health care challenges in the future, and we need to be prepared.”
Whatever comes, people need to talk about it like TB, Spanish Flu or other illnesses. Nurses need to learn more about the germ theory and look at evidence-based and scientific research studies. They need to look at data and statistics. After these interviews we walked around the hospital and saw positive things.
The nurses were proud of their “mini gown factory” and a wall where patients and staff write notes and posted cards of appreciation. These nurses are tough yet compassionate in dealing with the coronavirus and patients.
Ruth Bazhnibah Kawano is a retired registered nurse and a photographer, retired U.S. Public Health Service captain and a former captain in the U.S. Air Force.






 Highway 264,
Highway 264, I-40, WB @ Winslow
I-40, WB @ Winslow