
Vaccine reaches Western Navajo

Navajo Times | Krista Allen
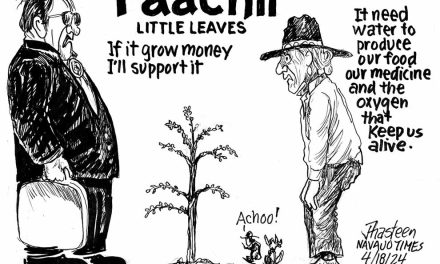
Clinical Nurse Practitioner Felicia French injects a patient with 0.3 ml of the Pfizer-BioNTech COVID-19 vaccine during a clinic outside the Warrior Pavilion in Tuba City on Friday, Jan. 15, 2021. A total of 760 people ages 65 years and over were vaccinated. Second doses were administered on Feb. 5, 2021.
By Krista Allen
Special to the Times
NAATSIS’ÁÁN-RAINBOW CITY, Utah
An 80-year-old woman was the first patient to be vaccinated at the Navajo Mountain Community Health Center on Jan. 5.
The woman, who arrived at the clinic with her grandson, received the Pfizer-BioNTech COVID-19 vaccine, which health care workers here say brings hope in small doses.
As Registered Nurse Modessa Hancock administered the shot, the woman talked about losing loved ones as a result of the pandemic. But she was excited and rejoiced in feeling one step closer to healing while she waited for observation following her vaccination.
“It was nice to see the smile on her face, and her grandson was with her,” lab technician Roxanna Yazzie said. “She’s hoping all this goes away because she lost a couple of her family members also.”
The vaccinations came just as the Navajo Nation reached 922 coronavirus deaths. The health care workers here, Yazzie says, found the gloom that has filled their small clinic since the pandemic replaced by elation. “I want to see a change in everything,” Yazzie said. “It’s really tough for all of us here at the clinic. In 2020, we lost really close elders who came here and who were regular patients …
“And we also lost other family members – it’s a small community,” she said. “If one person passes, it hurts the whole community.” Yazzie, along with her colleague Sonya Sloan, was vaccinated in Blanding, Utah, the day after Christmas. Their colleagues followed. “We were very anxious, we were nervous,” Yazzie said. “We talked about our family members and about the community members who passed on.”
Flagstaff Medical Center
Nurse Stacy Payne, who’s been treating COVID-19 patients in Flagstaff Medical Center’s critical care unit, rolled up her sleeves and waited for Nurse Practitioner Emilie Bowers to administer the Moderna COVID-19 vaccine. “I’m so ready! I’m so excited!” said Payne. “I feel like this is our whole planet coming together … to give us hope to get out of this (pandemic).”
Nurse Practitioner Nick Schumacher followed Payne. Schumacher, who’s part of the critical care provider team at FMC, leads the ICU and also treats COVID-19 patients. Dr. John Mougin, the chief quality officer for Northern Arizona Healthcare, said Schumacher had promised to wear a tuxedo with one short sleeve, but that didn’t happen because he was on the job when he received the vaccine.
“We’re all really excited about this,” Schumacher said. “We’ve been waiting for this day. We’re actually really excited that it’s happening as quickly as it is. We owe our thanks to the entire community that’s helped to develop and distribute these vaccinations. This is a great thing.”
Dr. Douglas W. Mapel was the third health care worker to receive the vaccine. He said he hopes the vaccine will start turning things around. “We can see some light at the end of the tunnel,” he said as he waited for Bowers to administer the vaccine and expected a Snoopy Band-Aid after the shot. “This is fantastic. I’ve participated in a number of vaccine studies before and in comparison to other things on the market, the efficacy of this is excellent.”
Mapel, who’s a pulmonologist and an internist at both FMC and Verde Valley Medical Center, said if people wait much longer to get the vaccine, thousands of people worldwide will die. “So the sooner we get everything on board and vaccinated, the faster we can get past this and get back to normal lives,” Mapel said, adding that the efficacy and safety of the Moderna COVID-19 vaccine, or mRNA-1273 SARS-CoV-2, are excellent.
The long-term studies, he says, are coming but people cannot afford to wait for long-term studies. “I agree,” Mougin said. “This is the first step, obviously with the vaccine in limited fashion. Even with the vaccine initially, we’re still recommending good COVID practices (such as) masking, physical distancing, and practicing good hygiene. When we get the vaccine in enough people, hopefully, that (masking and physical distancing) can go away – if we see the incidence of COVID drop or go away.”
The third health care worker who received the Moderna COVID-19 vaccine was Celeste Palmer, who works in FMC’s ICU. “I feel like this is the beginning of the stage for us to be able to start any type of normalcy,” she said. “It’s definitely going to help protect us.”
Vaccines won’t bring a quick end
The mood was downright giddy in Western Navajo when hundreds of health care and essential workers on the front lines, and people 65 years and older, received a COVID-19 vaccine in December and this month. But intensive care units in Arizona and across Utah Navajo remain near capacity and public health experts warn that life might not return to some sort of normalcy until next year.
“We will need to continue to use the precautions … for some time, even though the vaccine’s rolling out,” Mougin said. “And the reason behind this is really to keep our community safe.
It plays on several factors. First of all, we already see so many cases that hospitals are full across the state. It takes a while to get enough of the community vaccinated to get herd immunity.”
The coronavirus has had devastating consequences globally. Health experts at both Banner Health in Phoenix and Northern Arizona Health in Flagstaff say even though control measures have helped limit the transmission, vaccines are needed to reduce the morbidity and mortality associated with COVID-19. Mougin said the Moderna COVID-19 vaccine is a lipid nanoparticle-encapsulated messenger RNA-based vaccine that encodes the prefusion stabilized full-length spike protein of the coronavirus — meaning it’s not actually the virus.
“You cannot get infected from this,” Mougin said of the COVID-19 vaccine. “It’s not the virus itself, it’s just a small piece of it. It helps your immune system to fight off the live virus when it’s exposed to it. “So it’s a vaccine that induces cells in your body to produce a protein called the spike protein,” Mougin explained. “Your body then recognizes the spike protein as something that’s not supposed to be there, and it creates an immediate reaction against that.”
Mougin said this means if someone is exposed to the virus in the future, one’s body will recognize that quickly as being something that it needs to get rid of. And that creates the immunity.
Herd immunity, or community immunity, occurs when a high percentage of the community is immune to a disease – either through vaccination or prior illness, making the spread of the disease from person to person unlikely. Mougin said herd immunity is reached when at least 70% of the people are immune either by natural immunity or by vaccination.
Neither type of immunity makes you 100 percent impervious to the virus. “Even though you get the vaccine, you need to protect yourself until we really see the incidence of COVID-19 trailing off and reducing,” Mougin said, “which is a day I look forward to. Then we’ll know it’s time. Until then, we need to all continue to do our part as we’re still seeing a large number of cases.”
Health experts say the protective effects of vaccines are known to take at least a couple of weeks to kick in. “We now have an effective tool on our hands to combat the spread of COVID-19,” Mougin said. “It’s really the first step in getting back to some sense of our normal lives.”
High infections in Arizona
Arizona has remained one of the states with the highest COVID-19 infection rates in the country. “A conservative estimate suggests that about 1 in 10 Arizonans is currently infected with the virus,” said Dr. Marjorie Bessel, the chief clinical officer for Banner Health. “Cases, hospitalizations and deaths in our state continue to climb. Our reproduction rate remains above 1.0, which means the virus is spreading faster than desired.”
Bessel said hospitals in the state are under immense pressure as their leadership teams continue to expand capacity and adjust operations to accommodate a much higher volume and acuity of patients than they’re used to. Currently, 58% of hospital beds in Arizona are occupied by COVID-19 patients. And that percentage is even higher in state ICUs.
“These COVID-19 patients require much more attention and care than a typical ICU patient,” Bessel said. “From the start of the pandemic, Arizona hospitals and health systems agreed that we would work together,” explained Dr. Keith Frey, the chief medical officer for Dignity Health-Arizona Division.
“Arizona was one of the first states to stand up as a statewide surge line to ensure COVID-19 patients requiring hospitalization would have access to treatment at a health care facility with available capacity, and so that no one hospital or health system became overwhelmed.”
Frey said all of the hospital leaderships in Arizona also agreed that no hospital would activate the triage addendum of the Arizona Crisis Standards of Care plan (informally known as “rationing care”) unless all hospitals reached a critical shortage of life-saving resources.
The Arizona CSC Plan is a response and recovery framework for catastrophic disasters, such as the coronavirus pandemic. “This collaboration and commitment along with our respective systems’ efforts to scale up to meet the demand for health care services in our community are the reasons that we continue to be open and accessible for all those in need of care,” Frey added.
“I can tell you as a clinician, no provider ever wants to be in the position to implement something like this,” said Dr. Alyssa Chapital, hospital medical director for the Mayo Clinic in Phoenix. “We have all worked together since the start of the pandemic and we have developed a statewide triage plan that balances the load between our hospitals.”
Dr. Michael White, executive vice president and the chief clinical officer at Valleywise Health, said this is why more mitigation, more enforcement, and more personal commitment is needed to reduce the spread of COVID-19. “This means implementing additional measures like a statewide mask mandate, a curfew, stopping indoor dining, cancelling large gatherings, and adhering to a bi-directional roadmap for the opening and closing of businesses based on science and data,” White urged. “It also means that those rules must be enforced.”
As a public service, the Navajo Times is making all coverage of the coronavirus pandemic fully available on its website. Please support the Times by subscribing.
How to protect yourself and others.
Why masks work. Which masks are best.
Resources for coronavirus assistance





 Highway 264,
Highway 264, I-40, WB @ Winslow
I-40, WB @ Winslow